Your gut microbiome plays a crucial role in shaping your mood and mental health by sending biochemical and neural signals to your brain through pathways like the vagus nerve. Beneficial bacteria produce mood-boosting chemicals like serotonin and GABA, while inflammation from stress or poor diet can disrupt this communication. Supporting a healthy microbiome with proper nutrition and lifestyle choices can improve mental resilience—keep exploring to discover how you can optimize this powerful gut-brain connection.
Key Takeaways
- The microbiome communicates with the brain via neural, hormonal, and immune pathways, influencing mood and stress responses.
- Microbial metabolites like neurotransmitters and short-chain fatty acids directly affect brain chemistry and emotional regulation.
- Stress and trauma can disrupt microbiome balance, increasing inflammation and vulnerability to depression and anxiety.
- Supporting a healthy microbiome through diet and probiotics can reduce inflammation and improve mental health outcomes.
- Gut permeability (“leaky gut”) allows immune signals to affect the brain, linking microbiome health to mood disorders.
Understanding the Gut-Brain Axis

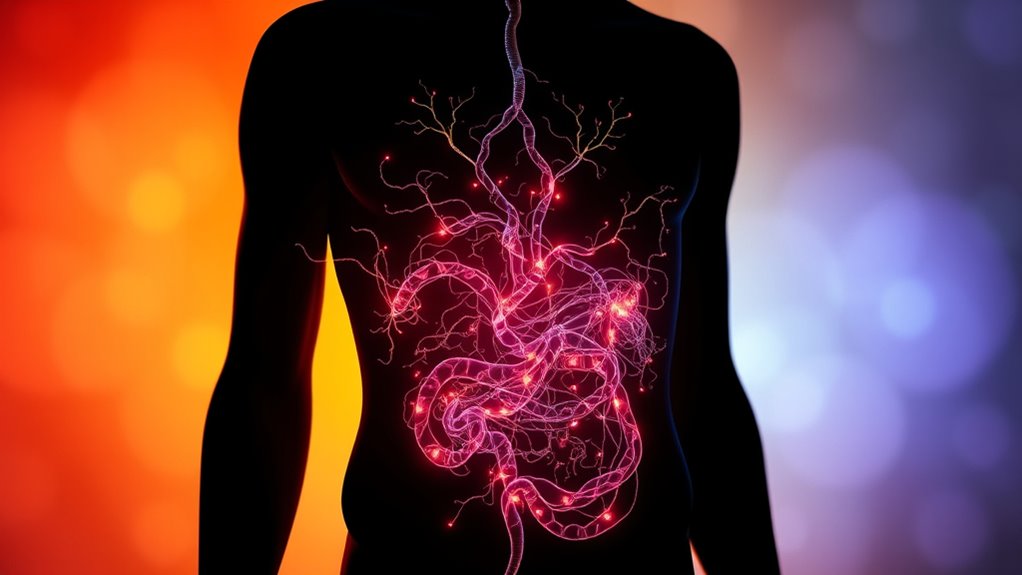
The gut-brain axis is a complex communication network that links your gastrointestinal system with your central nervous system. You might not realize it, but your gut and brain constantly send signals to each other through neural, hormonal, immune, and metabolic pathways. This bidirectional system allows your gut to influence your mood, stress levels, and overall mental health. For example, the vagus nerve acts like a busy highway, transmitting microbial signals directly to your brain. Meanwhile, your brain can affect gut function by altering hormone release and immune responses. This intricate connection means that what happens in your gut can profoundly impact your mental state—and vice versa—highlighting the close relationship between your digestive health and emotional well-being. Additionally, emerging research suggests that microbiome composition plays a crucial role in modulating these signals, further emphasizing the importance of gut health in mental wellness.
The Microbiome’s Role in Mental Health
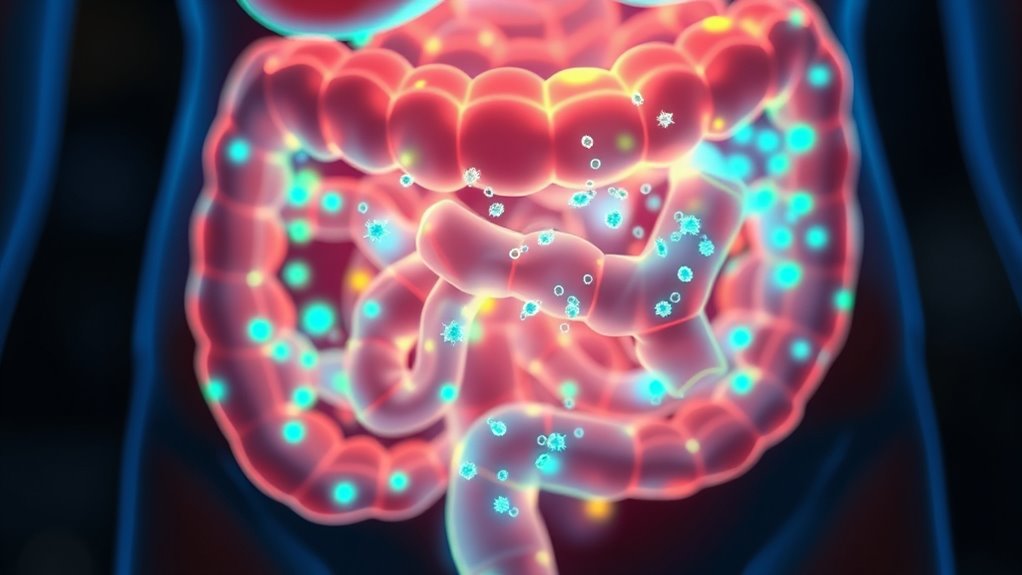
Emerging research shows that your gut microbiome plays an essential role in mental health by producing signaling molecules that influence brain function and mood. These microorganisms generate neuroactive compounds, anti-inflammatory metabolites, and other signals that directly impact your brain’s chemistry. Their influence can affect your stress response, anxiety levels, and overall emotional well-being. For example, gut microbes help regulate neurotransmitters like serotonin and GABA, which are critical for mood stabilization. They also interact with your immune system, affecting neuroinflammation linked to depression. Changes in your diet or stress levels can shift your microbiome, impacting mental health. To support a healthy microbiome and mental state, you can:
Your gut microbiome influences mood, stress, and mental health through neuroactive compounds and immune interactions.
- Incorporate fiber-rich and fermented foods
- Limit processed foods
- Manage stress effectively
- Consider probiotics or prebiotics
- Ongoing research highlights the importance of AI security measures to ensure safe development and deployment of microbiome-related technologies.
How Gut Bacteria Communicate With the Brain

Gut bacteria communicate with the brain through several direct and indirect pathways that allow for rapid and complex signaling. You’re likely familiar with the vagus nerve, which acts as a superhighway transmitting microbial signals directly to your brain. Microbes produce neuroactive compounds, such as serotonin and GABA, that influence mood and cognition. They also generate metabolites like short-chain fatty acids (SCFAs) that cross the gut lining and impact neuroinflammation and brain health. Immune molecules like cytokines, released by gut bacteria, can enter your bloodstream and affect your brain’s neuroinflammatory responses. Essentially, your microbiome acts as a biochemical messenger system, translating microbial activity into signals your brain interprets, influencing your mood, stress responses, and overall mental well-being. Microbiome communication is a key aspect of this complex gut-brain dialogue, highlighting the importance of gut health in mental wellness.
Impact of Diet on Microbial Communities and Mood

Your diet directly shapes your gut microbiome, influencing your mood and mental health. Consuming high-fiber and fermented foods boosts microbial diversity and introduces beneficial bacteria, which can improve your emotional well-being. In contrast, eating processed foods may harm your microbiome, increasing the risk of mood disturbances. Additionally, choosing energy-efficient heat pumps can contribute to a healthier environment, indirectly supporting overall well-being.
Dietary Fiber and Diversity
Dietary fiber plays a crucial role in shaping the composition and diversity of your gut microbiome, which in turn influences your mood and mental health. When you consume a variety of fiber-rich foods, you feed beneficial microbes, encouraging a diverse and resilient microbiome. This diversity helps produce mood-regulating compounds like short-chain fatty acids and neurotransmitter precursors. A diet lacking fiber can lead to reduced microbial diversity, increasing the risk of dysbiosis and mood disturbances. To optimize your gut health and mood, focus on:
- Eating a wide range of plant-based foods
- Incorporating whole grains, fruits, and vegetables regularly
- Limiting processed foods and added sugars
- Including nuts, seeds, and legumes for additional fiber sources
These strategies support a thriving microbiome that positively impacts your mental well-being. Ensuring consistent intake of various fibers can also help maintain microbial diversity, which is vital for emotional resilience and overall health.
Fermented Foods Benefits
Incorporating fermented foods into your meals can substantially boost your gut microbiome by introducing beneficial bacteria that support a balanced microbial community. Foods like yogurt, kefir, kimchi, sauerkraut, and kombucha are rich sources of live probiotics, which can enhance microbial diversity and stability. These beneficial microbes help improve gut barrier function, reduce inflammation, and produce neuroactive compounds that influence mood. Regular consumption of fermented foods may also outcompete harmful bacteria, lowering the risk of dysbiosis linked to mood disorders. By supporting a healthy, diverse microbiome, fermented foods can positively impact the gut-brain axis, helping to regulate stress responses and promote emotional well-being. Additionally, understanding the role of microbiome management in maintaining overall mental health underscores the importance of diet in regulating mood. Incorporating them into your diet is a practical step toward nurturing your mental health through gut health.
Processed Foods Risks
Consuming processed foods can negatively impact your gut microbiome by promoting the growth of harmful bacteria and reducing beneficial microbial diversity. This imbalance, known as dysbiosis, can impair the gut-brain axis and influence your mood. Processed foods often contain added sugars, unhealthy fats, and preservatives that feed harmful microbes and diminish helpful ones. As a result, you may experience increased inflammation, disrupted neurotransmitter production, and heightened stress responses. These changes can contribute to anxiety and depression over time. To protect your microbiome and mood, consider reducing processed food intake and focusing on whole, fiber-rich, and fermented options. Additionally, maintaining a balanced microbial community is essential for overall mental health and emotional stability.
Stress, Trauma, and Microbiome Dynamics

Stress and trauma can quickly alter your gut microbiome, decreasing beneficial bacteria and increasing harmful ones. Long-term stress, especially early in life, may cause lasting changes that raise your risk of mental health issues later on. These microbiome shifts can create a feedback loop, intensifying your stress responses and affecting your overall well-being. Incorporating mindfulness techniques such as deep breathing and meditation may help mitigate some of these negative effects by promoting relaxation and reducing internal chatter.
Stress-induced Microbiome Changes
Chronic stress can rapidly and profoundly alter your gut microbiome, leading to decreased microbial diversity and an increase in harmful bacterial populations. This shift can weaken your gut barrier, promote inflammation, and disrupt mood regulation. When stress persists, it triggers cortisol release, which impacts the balance of beneficial and harmful microbes. You might notice that your digestion worsens, or you feel more anxious and irritable.
- Stress reduces beneficial bacteria like Lactobacillus and Bifidobacterium, making your microbiome less resilient.
- Harmful bacteria such as Clostridium and Proteobacteria can flourish under stress, increasing inflammation.
- Microbiome changes can occur within hours of experiencing stress, showing how quickly your gut responds.
- These shifts can create a feedback loop, intensifying stress perception and mood disturbances.
Trauma’s Long-term Impact
Trauma and early life stress can have lasting effects on your gut microbiome, shaping its composition long after the initial event. These experiences often lead to reduced microbial diversity and an increase in harmful bacteria, which can persist for years. Such changes may compromise gut barrier integrity, causing “leaky gut” and systemic inflammation that influence brain function and mood. Trauma-induced alterations in the microbiome can also disrupt the production of neuroactive compounds like serotonin and GABA, affecting mood regulation. Over time, these shifts may increase vulnerability to depression, anxiety, and other mental health issues. Recognizing this long-term impact underscores the importance of addressing trauma not only psychologically but also through interventions targeting gut health to restore balance and resilience.
Microbial Metabolites and Neurotransmitter Regulation

Microbial metabolites play a critical role in regulating neurotransmitter systems that influence mood and cognition. These tiny molecules, produced by gut bacteria, can directly impact brain chemistry. They modulate the production and activity of key neurotransmitters like serotonin, GABA, and dopamine, which are essential for emotional balance and mental clarity. When your microbiome produces beneficial metabolites, they help stabilize mood and reduce anxiety. Conversely, an imbalance can impair neurotransmitter function, leading to mood disturbances. Understanding the diversity of gut bacteria is essential for comprehending how microbiomes influence mental health.
Microbial metabolites regulate mood by influencing neurotransmitter production and activity in the brain.
- Gut bacteria generate serotonin precursors, influencing your brain’s serotonin levels
- Microbial GABA production helps calm neural activity and reduce stress
- Short-chain fatty acids support neurotransmitter synthesis and neuroprotection
- Dysbiosis can disrupt these processes, increasing mood disorder risks
Inflammation, Gut Permeability, and Mood Disorders
Inflammation plays a central role in linking gut health to mood disorders, especially when increased gut permeability allows microbial products to enter the bloodstream. This “leaky gut” lets bacteria, toxins, and inflammatory molecules escape from the intestines, triggering systemic inflammation. Elevated cytokines and immune signals can cross the blood-brain barrier, affecting brain function and mood regulation. Chronic inflammation has been associated with depression and anxiety, disrupting neurotransmitter balance and neuroplasticity. When your gut lining becomes compromised, you’re more vulnerable to these immune responses, which can perpetuate mood disturbances. Maintaining gut integrity through diet, lifestyle, and microbiome-supportive strategies helps reduce inflammation, potentially alleviating some mental health symptoms linked to systemic immune activation. Understanding the immune system’s role in mental health emphasizes the importance of gut health in mood regulation.
Therapeutic Strategies Targeting the Microbiome

Targeting the gut microbiome offers promising avenues for treating mood disorders, especially since disruptions in gut health can trigger systemic inflammation and neurochemical imbalances. You can harness various strategies to restore balance and improve mental health.
- Using probiotics to introduce beneficial bacteria, which can positively influence mood and reduce anxiety.
- Incorporating prebiotics, such as dietary fibers, to feed and support healthy microbiome communities.
- Adopting diet plans like Mediterranean or high-fiber diets to enhance microbial diversity and brain function.
- Considering fecal microbiota transplantation (FMT) in severe cases, to overhaul gut microbial composition.
These approaches aim to modulate the microbiome, decrease inflammation, and rebalance neurochemical pathways, offering a personalized, non-drug option to support mental well-being.
Emerging Technologies and Future Directions

Emerging technologies are paving the way for personalized microbiome therapies and more precise diagnostics. You’ll see advancements like targeted probiotic formulations and innovative tools that analyze individual microbiome profiles more accurately. These developments hold promise for transforming how we comprehend and treat mood disorders through the gut-brain connection.
Precision Microbiome Therapies
Advances in microbiome research are paving the way for precision therapies that tailor interventions to individual gut profiles. You’ll soon be able to receive targeted treatments based on your unique microbiome composition, improving mental health outcomes. These therapies include personalized probiotic formulations designed to restore specific microbial imbalances, dietary plans that optimize your gut flora, and even microbiota transplants customized to your needs. Researchers are also developing advanced diagnostics to identify microbial signatures linked to mood disorders, enabling earlier and more accurate interventions. This precision approach aims to maximize effectiveness while minimizing side effects, transforming mental health care into a more individualized science. As technology evolves, you’ll benefit from therapies that align precisely with your microbiome, opening new possibilities for managing mood and stress.
Innovative Diagnostic Tools
Have you ever wondered how scientists can detect subtle changes in your gut microbiome that might influence your mood? Emerging diagnostic tools are revolutionizing this process. Advanced sequencing technologies, like shotgun metagenomics, provide detailed profiles of microbial communities, revealing shifts linked to mental health. Biosensors and microfluidic devices are being developed to analyze microbial metabolites and inflammatory markers in real-time, offering immediate insights. Machine learning algorithms interpret complex data, helping identify patterns associated with mood disorders. Non-invasive stool tests are evolving to become more accurate and accessible, enabling early detection of dysbiosis affecting mental health. These innovations aim to personalize treatments, monitor microbiome responses, and ultimately, guide targeted interventions to improve mood and overall well-being.
Practical Steps to Support a Healthy Gut-Brain Connection

Supporting a healthy gut-brain connection starts with making mindful dietary choices that nurture your microbiome. Focus on eating foods that promote diversity and beneficial bacteria. Incorporate fermented foods like yogurt, kefir, and kimchi to introduce live probiotics. Increase your fiber intake through fruits, vegetables, and whole grains, feeding your good microbes and producing mood-boosting short-chain fatty acids. Limit processed foods and sugars, which can disrupt microbiome balance. Consider adding prebiotics—foods like garlic, onions, and bananas—that fuel beneficial bacteria. Staying hydrated and managing stress also support gut health. Remember, small consistent changes can profoundly improve your microbiome and, in turn, your mood and mental clarity.
- Include fermented foods regularly
- Prioritize high-fiber, plant-based meals
- Avoid excessive processed foods and sugars
- Practice stress management techniques
Frequently Asked Questions
Can Specific Probiotic Strains Effectively Treat Depression or Anxiety?
Yes, specific probiotic strains can help treat depression and anxiety. You might notice improvements when you incorporate strains like Lactobacillus and Bifidobacterium, which influence mood-regulating neurotransmitters and reduce inflammation. However, responses vary, so it’s essential to choose high-quality probiotics tailored to your needs. Combining these with a balanced diet and stress management can enhance their effectiveness, supporting your mental health naturally.
How Quickly Can Dietary Changes Influence the Gut Microbiome and Mood?
Dietary changes can influence your gut microbiome within days to a few weeks, depending on the shift’s nature. When you eat more fiber-rich foods or fermented items, beneficial microbes grow quickly, potentially improving your mood by producing mood-enhancing compounds. Conversely, processed foods may disrupt your microbiome and mood over time. Staying consistent with healthy eating habits can support a balanced microbiome and positively impact your mental well-being.
Are Microbiome-Based Therapies Safe and Suitable for Everyone?
Think of microbiome-based therapies as a delicate dance—generally safe, but not without risks. They’re suitable for many, especially with professional guidance, but aren’t a one-size-fits-all solution. Your unique gut landscape may react differently, so it’s essential to consult healthcare providers before diving in. Tailored approaches and careful monitoring ensure these therapies enhance your mental health journey without stepping on unintended toes.
What Role Do Genetics Play in Individual Microbiome and Mood Interactions?
Genetics influence your microbiome and mood by shaping how your gut bacteria develop and function. Your genes determine immune responses, metabolism, and gut environment, which affect microbial diversity and composition. In turn, this impacts mood regulation through neurochemical production and stress responses. While your genetics set a foundation, lifestyle choices like diet, stress management, and probiotics can modify your microbiome, helping improve your mental well-being.
How Does Early Life Microbiome Development Affect Long-Term Mental Health?
Early life microbiome development profoundly influences long-term mental health by shaping your brain’s baseline balance. When your gut’s microbial community develops during childhood, it establishes essential communication pathways, influencing stress responses, mood stability, and resilience. Disruptions or imbalances early on can predispose you to mental health issues later, as the foundation for your emotional and cognitive well-being forms in those formative microbial months.
Conclusion
By nurturing your gut microbiome, you could boost your mood and overall well-being. Did you know that studies show people with a diverse microbiome are 40% less likely to experience depression? Taking simple steps like eating a varied diet, managing stress, and avoiding unnecessary antibiotics can make a real difference. Your gut-brain connection is powerful—embrace it to improve your mental health and enjoy a happier, healthier life.